
Use of injection techniques in orofacial pain emergencies: a narrative review
Introduction
The term ‘urgent care’ as defined by the Merriam-Webster medical dictionary is a ‘medical care provided for illnesses or injuries which require prompt attention, but are typically not of such seriousness as to require emergency services’. Quite simply, it means an urgent need for assistance or relief. In dentistry, most dental emergencies are due to dental abscesses, tooth decay or fracture of dentition (1). Orofacial pain is that specialty of dentistry that deals with jaw, face, head and neck pain of non-odontogenic origin (2) and as such, it is not immune to patients presenting with an urgent situation in extreme pain, requiring the practioner to provide efficient and effective care.
Orofacial Pain can be broadly divided into temporomandibular, neuropathic, and neurovascular disorders. The reader is urged to refer to the International Classification of Orofacial Pain (ICOP 2020) and the DC-TMD for the official diagnostic criteria (3). It is important to always keep in mind that dental pathology should be ruled out first before looking for an orofacial pain diagnosis, as dentoalveolar pathology is the most common cause of pain in the orofacial region (3). Another important point to keep in mind is the site of pain versus the source of pain. The site of pain is the location where the patient feels the pain. The source of pain is that area of the body from which the pain actually originates. The term primary pain is used, if the site and source of pain are the same. If the site and source of pain are different, it is called as heterotopic pain. Referred pain is a type of heterotopic pain. An important rule of thumb in therapy is that treatment should be directed toward the source and not the site of pain (4).
Injection therapy can be used as a tool for the diagnosis and management of urgent orofacial pain conditions. Injections can be performed without any injectates (dry needling) or with various injectates such as local anesthetics, corticosteroids, and botulinum toxins (5). Local anesthetics are the most common injectable drugs, used in emergency/urgent setting. There are reports on the effective use of local anesthetic injections for confirming a diagnosis, and in the management of intolerable pain (6). The advantages of injection therapy with local anesthetics include ease of administration, achieving immediate pain relief with minimal side effects. It is thought that local anesthetics reduce the pain transmitting signals from the periphery, by anesthetizing the sensitized, pain producing nerves- specifically the C-fibers (6). The objective of presenting this timely review, is to concisely summarize the common urgent presentations in an orofacial pain setting and how to provide immediate pain relief by performing various injection techniques. We present the following article in accordance with the Narrative Review reporting checklist (available at https://joma.amegroups.com/article/view/10.21037/joma-22-11/rc).
Methods
Please see Table 1 for the search strategy summary. The search was conducted on PubMed database. English language articles were included. The search was conducted with the MeSH terms: injections, neuralgia, TMJ disorders, local anesthetics, cluster headache, migraine headache. In addition, the cited manuscripts were reviewed.
Table 1
| Items | Specification |
|---|---|
| Date of search | January 9, 2022 |
| Databases and other sources searched | PubMed |
| Search terms used | Injections, neuralgia, TMJ disorders, local anesthetics, cluster headache, migraine headache. In addition, the cited manuscripts were reviewed |
| Timeframe | January 9, 2022 to June 1, 2022 |
| Inclusion and exclusion criteria | English language publications were included |
| Selection process | Dr. Gomes Zagury & Dr. Ananthan; Consensus was obtained by cross verifying the references |
TMJ, temporomandibular joint.
Rationale for the review
Urgent situations in orofacial pain can present with unremitting pain or excruciating intermittent pain that requires effective and rapid treatment. This can be achieved with different injection techniques, either with or without the use of injectables. This will help the patient until further interventions can be performed or until therapeutic dose of the prescribed medications is reached. Different injection techniques for urgent care in an orofacial pain setting will be discussed based on the literature.
Therapeutic drugs
Local anesthetics
Modern dentistry will be impossible without this wonder medication (7). Local anesthetics reversibly interrupt neuronal conduction by blocking sodium channels within the neuronal membranes. The smaller nerve fibers are more susceptible to local anesthetics than the larger diameter nerve fibers. The pain conducting C- and A delta fibers are blocked first and then the larger diameter A beta and A alpha fibers. Local anesthetics vary in their potency, depending on their lipid solubility. The greater the lipid solubility, the greater the potency of the local anesthetic. Lidocaine, an amide type local anesthetic, is the gold standard local anesthetic. In concentrations up to 2% without the vasoconstrictor, it provides sufficient, fast, short-lasting anesthesia. Lidocaine’s efficacy is improved when combined with a vasoconstrictor (8,9). Mepivacaine has milder vasodilator properties but has a longer duration of action when used without a vasoconstrictor. In dentistry, this is available as a 3% solution without a vasoconstrictor or a 2% solution with a vasoconstrictor. Vasoconstrictor containing anesthetic solutions should be generally avoided in muscle injections, to prevent vasoconstriction as circulation may already be compromised due to on-going muscle contraction or spasm. Bupivacaine is a long-acting local anesthetic, however, is extremely myotoxic. It has a specific destructive effect on the adult skeletal muscle fibers (10) and is used primarily for spinal anesthesia. It should also be noted that Bupivacaine exhibits a greater potential for direct cardiac toxicity than other local anesthetics, and renders the cardiac tissues more susceptible to developing arrhythmias (11). Articaine is a safe and efficacious local anesthetic for routine dental procedures for all age range of patients. The onset and duration of anesthesia is faster than that of lidocaine for buccal infiltrations (12). However, when used for mandibular nerve blocks, paresthesia was found to be at least 2 times likely with 4% articaine, as compared to 4% prilocaine (11). Skeletal muscle injections can result in myotoxicity, which can be reversible due to muscular regeneration in 3–4 weeks (13), which suggests that injections of local anesthetics into the muscles should not be done very often, though more studies are needed on this subject.
Complications arising from peripheral nerve blocks are usually mild and transient. They include dizziness, vertigo, pain at the injection site, toxicity-if the volume of anesthetic solution is considerable or if there is inadvertent intravascular injection, or if injections are given more frequently than when the muscle is able to regenerate, allergic reaction, methemoglobinemia, and depending on the site of administration—transient facial nerve palsy, pneumothorax, or subarachnoid injections. Additionally, direct, or indirect neural trauma may occur during the injection process. Indirect nerve injury may occur due to local edema or hematoma with resulting ischemia (14). Caution is advised in cases of cardiac transplant, pregnancy, use of anti-thrombotic agents as well as presence of systemic or local infections (14,15).
Corticosteroids with local anesthetics
Corticosteroids may be used in conjunction with local anesthetics in patients with post-herpetic neuralgia, trigeminal neuropathy secondary to a traumatic neuroma, cluster and cervicogenic headaches. Commonly used corticosteroids are dexamethasone, triamcinolone, and betamethasone. Caution is advised in patients with diabetes and glaucoma. Adverse events such as local alopecia and skin lightening may occur after steroid injections (16). Multiple injections are discouraged due to increased risk of systemic side effects. Locally, corticosteroids reduce peripheral afferent sensitization through an anti-inflammatory effect, in addition, to having adjuvant analgesic effects (17). Based on a randomized controlled trial, steroids do not seem to have clinical relevance on extending the effect of the local anesthetic (18).
Collagen injections
Collagen is a molecule in the extra cellular matrix that plays an important role in building networks in the skeletal muscle. This is a novel injection therapy using muscle collagen for myofascial pain. The results are promising as shown in a recent randomized clinical trial, when compared to lidocaine and saline injections (19). There was a significant reduction of moderate to severe myofascial pain with repeated injections, but there was an increase in pain level and edema within 30 min of the injections that subsided within an hour (19).
There are additional injection modalities described in the literature for the management of different orofacial pain conditions, such as intra-articular or intra-muscular platelet-rich plasma for myofascial pain, intraarticular hyaluronic acid injections for friction related dysfunction such as frequent and painful internal derangements, osteoarthritis, dextrose prolotherapy for osteoarthritis and tendinopathies. Since they are used in chronic pain settings, they will not be included in this review.
A note on Botulinum toxin
Botulinum toxin type A (BoNT-A) produces a sustained and prolonged relaxation of muscles by inhibiting the release of acetylcholine at the motor end plate and is analgesic, wherein it is believed to inhibit central sensitization. Several studies have shown the efficacy of botulinum toxin to be superior to that of local anesthetics and steroids (5) and that it may be useful for patients with myofascial pain syndrome, resistant to conventional treatment, i.e., it is typically not used in acute situations. Though Botulinum toxin treatment is generally well tolerated, they do have adverse effects, such as temporary regional weakness, tenderness over the injection sites. In some situations, an asymmetric smile or reduction in muscle size, paresthesia, eye drooping, weakness, speech changes and bruising, among others, may be seen (20).
Orofacial pain emergencies
Dental emergencies
Dental pain originating primarily from the tooth pulp and/ or the surrounding periodontium may present with clinical or radiographic evidence of a lesion or traumatic injury. When examining these patients’ various diagnostic modalities such as percussing the involved tooth, thermal challenge (e.g., heat or cold), chemical (e.g., sweets) and the electric pulp test should be considered. A cracked tooth may present with symptoms manifesting as sharp pain on biting down, pain on release of the biting pressure along with cold hypersensitivity. If the source for the discomfort is not clear, a simple local anesthetic infiltration or block can aid in making a diagnosis. Another important point to remember is that when the symptoms are nebulous, it is better to wait and watch. A toothache of dental origin will always show itself eventually. Patients may present with an urgent situation, with acute dental infection for emergency analgesia, especially if they have limited access to dental services and dental phobia (21). Since all dentists are trained extensively in giving infiltrations and nerve blocks to block specific teeth as necessary, they will not be described exclusively in this review.
Temporomandibular disorders (TMDs)
TMDs are a collective term used to describe several painful and non-painful conditions affecting the temporomandibular joints (TMJs) and its associated structures and the musculature. As per the diagnostic classification for TMDs, they are broadly classified as arthrogenous and myogenous TMDs. In this review, we will discuss, a common cause of arthrogenous TMD emergency—acute disc displacement without reduction, and luxation (open lock), myogenous TMD emergencies include: an acute elevator muscle spasm and severe myofascial pain.
TMJ pain attributed to disc displacement without reduction
One of the common arthrogenous TMD emergencies is an acute disc displacement without reduction with limited mouth opening. The ICOP defines this, with the following criteria—jaw locked or caught, so that full opening is prevented and there is limitation of jaw opening, with interference present while eating. This occurs when the fibrocartilaginous TMJ disc is unable to return to its position between the condyle and the fossa. Consequently, the nerves and the blood vessels within the retro discal tissues are compressed over the head of the TMJ. In an acute situation, this can be extremely painful, and the patient can present to the dental practitioner with severe pain and limited mouth opening. In this situation, attempts to ‘reduce’ the displaced disc may be hampered by the patient’s acute pain. In this scenario, the auriculotemporal block, the temporo-masseteric nerve block (22) can be administered in order to reduce the pain from manipulation.
Painful internal derangement can be accompanied with a painful elevator muscle spasm, including the lateral pterygoid muscle (injection technique described under the section on secondary myofascial pain). In both conditions, mouth opening is limited with a deflection of the mandible to the affected side. The ICOP defines this as pain reported in the jaw, temple, ear or in the preauricular region, with confirmation on examination, there is provocation of pain by palpation of the affected tendon/s and/or maximum unassisted or assisted jaw opening movements. The differential diagnosis of muscle vs. joint is explained in Table 2. Once the patient is pain free from the nerve block, an attempt can be made to ‘reduce’ the disc by placing the operator’s thumb on the most posterior molar and depressing the mandible and moving it to the opposite side, to manually provide space for the disc to get back into the ‘normal’ position. The patient is encouraged to take a soft diet, use heat application, massage, limiting the range of motion, taking non-steroidal anti-inflammatory medications, and physical therapy (23), along with fabrication of an emergency appliance (24).
Table 2
| Parameter | Myofascial orofacial pain attributed to muscle spasm | TMJ pain attributed to disc displacement without reduction |
|---|---|---|
| Range of motion | Generally, <20 mm | Generally, >20 mm |
| Gait of mandible | Deflection to ipsilateral side on opening (exception: medial pterygoid muscle) | Deflection to ipsilateral side on opening |
| End feel | Soft | Hard |
| Lateral excursions | Similar | Limited to the contra-lateral side |
TMJ, temporomandibular joint.
TMJ pain attributed to subluxation
TMJ pain can be attributed to subluxation, where there is a history/instance of jaw locking or catching, preventing the closure from the wide-open position. The patient will complaint of an inability to close the mouth, without a specific manipulative maneuver (3). It results usually in an acute situation, as the surrounding tissues are overstretched and the muscles may go into a state of spasm. In this situation, the patient may derive benefit from a temporo-masseteric nerve block, which will anesthetize the joint as well as the temporalis and masseter muscles, or the auriculotemporal nerve block which has the effect of anesthetizing the joint and helping the patient to relax so that the manipulative maneuver can be accomplished.
Auriculotemporal nerve block (23) (Figure 1)
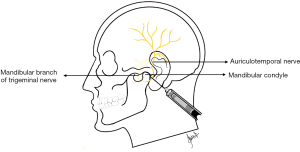
The mandibular condylar is palpated by asking the patient to open and close their mouth. The patient is asked to then close their mouth into occlusion, a 35-mm long and 0.5 mm diameter needle is inserted about 6 mm anterior to the tragus, and is directed posteriorly toward the condylar neck, and upon touching bone to a depth of 25–28 mm, about 0.5 mL of the local anesthetic is injected into the periarticular tissues (25). Either 2% Lidocaine or 3% Mepivacaine without vasoconstrictor can be used for this block.
Temporo-masseteric nerve block (previously called the Twin Block) (Figure 2)
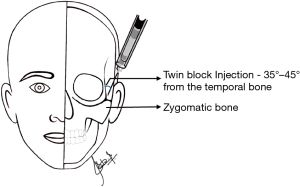
The point of entry of a 27-gauge long needle is 1 cm behind the orbital rim and 1 cm above the zygomatic arch at an angle of 35–45 degrees from the temporal bone and perpendicular to the zygomatic process (26). The temporo-masseteric nerve block is useful for reducing a painful non-reducing disc as well (22). The whole carpule (1.8 mL) of 2% Lidocaine with or without vasoconstrictor can be used for this block.
Acute primary myofascial orofacial pain
The ICOP defines this condition as mild to moderate levels of deep aching or pressing pain in the masticatory muscles, occurring episodically or unremittingly. Patients experience perceived difficulties in moving the lower jaw, chewing and/or yawning. The onset should have been within the last 3 months. The pathophysiology of myofascial pain is not fully understood and detailed discussion on it is beyond the scope of this manuscript. Multiple central and local factors are involved. Simons and colleagues have developed a set of diagnostic criteria that are used for locating the trigger points. These include: palpating the taut band of muscle, tenderness from the taut band, pain reproducibility, local twitch response, limited range of motion, and referral of pain (5).
In this situation, once the diagnosis is confirmed with digital palpation, the temporo-masseteric nerve block can be administered. Alternately, a trigger point injection can be given with either 2% lidocaine or 3% mepivacaine without vasoconstrictor. Another choice can be the masseteric nerve block if the masseter muscle alone is involved.
Technique for the masseter muscle trigger point injection
Palpation of masseter and temporalis muscles is performed by the flat palpation technique. This trigger point area is isolated between the fingers after the area has been cleaned with betadine and alcohol. A 30-gauge short needle is inserted until bone is touched, slightly withdrawn and the area is ‘peppered’ with the needle and the local anesthetic solution. The use of local anesthetics in this situation is advantageous, to break the cycle of pain the patient has been experiencing and to reduce the post-injection soreness from the needling technique. It should be pointed out that the temporo-masseteric nerve block has been shown to be efficacious in managing myofascial pain arising from both the temporalis and masseter muscles, as compared to the traditional trigger point injections (27). This technique has been described above.
Masseteric nerve block (Figure 3)

This is an effective technique for anesthetizing the masseter muscle. When the mandibular division of the trigeminal nerve exits the skull through the foramen ovale, the anterior division of V3 along with the masseteric nerve passes through the infratemporal fossa, and the masseteric nerve passes through the sigmoid notch to innervate the masseter muscle (28). The anterior and posterior borders of the ramus are palpated between the thumb and the middle finger, while the index finger traces the mid-point and travels superiorly to palpate the sigmoid/ mandibular notch. A 27-gauge, long needle is used, and half the length is inserted into the sigmoid notch to deposit the anesthetic solution. Either Lidocaine or Mepivacaine can be used for this block.
Intramuscular collagen injection
The protocol suggested for intramuscular collagen injection for myofascial pain is based on the procedure described by Nitecka-Buchta et al. The most tender muscle trigger point through palpation of the muscle is identified and after sanitizing the skin, the region of the trigger point is held between two fingers (thumb and index finger/index finger and middle finger). Using a short (19 mm) 27-guage needle, the authors of the study injected 2 mL of Collagen MD muscle (Guna, Italy) into the trigger point to about 1 to 1.5 cm of penetration (19).
Secondary myofascial orofacial pain
Secondary masticatory myofascial pain may occur secondary to infection, inflammation, or muscle spasm. The pain can be located at the jaw, temple, ear and/or pre-auricular region, and can be reproduced either by palpation of the affected muscle(s) or tendon(s) or provoked during maximum mouth opening (3). Inflammation, infection and trauma of the masticatory muscles may result in intense pain and patients may be unable to open their mouth. A closed-mouth anesthetic block technique, such as Vazirani-Akinosi technique, may assist these patients in the emergency setting, as long as the area to be injected has no infection.
The temporal tendon is an enthesis—i.e., the site of insertion of the temporalis muscle onto the coronoid process of the mandible. Enthesitis i.e., inflammation of the enthesis can cause localized facial pain, inferior to the region of the mid-zygomatic arch, with referrals to the TMJ area, the eye, ear and maxillary teeth (29). Injecting this tendon can help to eliminate the temporal tendon as a source of pain, giving significant pain relief to patients.
In cases of myofascial pain secondary to tendonitis, concomitant muscle pain will improve with the resolution of the tendonitis (3). Therefore, temporal tendon block may assist in the diagnosis and will provide pain relief.
Vazirani-Akinosi technique (Figure 4)

In an orofacial pain emergency, anesthesia of the inferior alveolar nerve may be required in a patient with trismus, who is unable to open his/her mouth. The Vazirani-Akinosi technique is an intraoral closed-mouth technique that blocks sensory and motor innervation of the mandibular branch (inferior alveolar and terminal branches, lingual, mylohyoid nerves), reducing pain and relieving trismus (30).
The patient stays with teeth occluded and muscles relaxed, and the syringe is placed parallel to the occlusal plane and tangent to the maxillary alveolar arch ipsilateral to the nerve to be anesthetized. After reflecting the buccal mucosa laterally to allow better visualization, a 25- or 27-gauge long needle, with the bevel directed towards the midline is inserted into the mucogingival junction of maxillary third or second molars. The penetration of the needle is of 25 mm from the maxillary tuberosity (30). The main disadvantage of this technique is that there is uncertainty around the needle tip localization as there is no bony contact with any structure (31).
Temporal tendon injection technique
The temporal tendon is palpated by running the index finger on the anterior border of the ramus of the mandible, to the most superior area. Palpating this area should reproduce the patient’s complaint of familiar pain. Using a 27-gauge 40 mm long needle, either 3% Carbocaine without epinephrine or 2% Lidocaine with or without epinephrine can be injected (32). The authors feel that a useful landmark for this technique is using the mesio-buccal cusp of the second maxillary molar and to direct the needle laterally toward the coronoid process. Half to three fourths of the needle length is inserted and after aspiration, the local anesthetic solution is slowly injected. If correctly done, this injection immediately will alleviate the patient’s pain complaint.
Lateral pterygoid muscle injection
The lateral pterygoid muscle can be injected via either the extra-oral or intra-oral approaches. For the intra-oral approach, the needle needs to be inserted at least 1 inch, into the muscle, by inserting lateral to the sigmoid notch of the mandible, after asking the patient to move the mandible laterally to provide access for the needle entry into the muscle. Only the inferior belly of the muscle will be accessible from the intraoral approach. It should be pointed out that the intra-oral technique is a blind injection and is difficult to standardize, not to mention dangerous as risk of neurovascular injury is increased (33). This injection should be done under electromyographic guidance, though multiple authors have described standardized, extra-oral injection techniques for the lateral pterygoid muscle (33,34).
Orofacial pain attributed to lesion or disease of the cranial nerves
The International Association for the Study of Pain defines neuropathic pain as pain caused by a lesion or disease of the somatosensory nervous system (35). As stated by the IASP, it is not a diagnosis, but a clinical description of different conditions. The ICOP included orofacial pain conditions attributed to a lesion or disease of two cranial nerves, the trigeminal and glossopharyngeal. Conditions affecting the trigeminal nerve broadly include trigeminal neuralgia (TN) and trigeminal neuropathic pain. Urgent care in an orofacial pain setting may be required for patients with TN and those who may suffer with severe pain exacerbation from trigeminal neuropathy, though by nature, these are chronic pain conditions. Peripheral nerve injections may aim to anesthetize the trigger zones in TN.
Neuralgia is defined as ‘pain in the distribution of a nerve or nerves’ (35). In general, features of neuralgic pain include excruciating electrical intermittent paroxysmal pain, triggered by innocuous stimulation. Pain location follows the distribution of the nerve involved. Pain management can be delayed due to slow titration of medications, sometimes patients can be unresponsive, or develop side effects.
TN
The trigeminal nerve divides peripherally into three major branches—the ophthalmic, maxillary, and mandibular branches. TN affects the second and third divisions more frequently (36). About half of patients with TN, present with extra or intraoral trigger zones (37), which are areas when touched with innocuous stimuli, trigger the severe pain associated with TN. In cases recently diagnosed or refractory to treatment, local anesthetic blocks can provide immediate pain relief and give the patient a respite from the pain and can help patients to perform activities of daily living, such as eating, drinking, and brushing their teeth (38,39). When the third division of the trigeminal nerve is affected, the inferior alveolar nerve block (IANB), Gow-Gates or Vazrizani-Akinosi techniques can be used. If the second division is affected, various techniques such as local infiltrations (i.e., supraperiosteal injections), infraorbital nerve block, posterior superior alveolar nerve block or maxillary nerve block sphenopalatine ganglion blocks can be used.
Supraperiosteal injections using local anesthetics
Supraperiosteal injections are simple to perform, and they have a rapid onset (within 5 minutes) and are highly successful (31). They anesthetize terminal branches of the sensory nerve that supply one to a few teeth and the surrounding soft tissue. To anesthetize mandibular teeth, local anesthetics with greater penetration capacity, such as 4% articaine show greater efficacy as compared to 2% lidocaine.
A short 27-gauge needle can be used and placed parallel to the long axis of the tooth with the bevel directed to the alveolar bone. The needle penetrates the muco-buccal fold a few millimeters towards the apex of the tooth, where the anesthetic solution is slowly delivered following aspiration. Whenever possible, the bevel of the needle should face the bone. For detailed maxillary and mandibular regional nerve block techniques, the reader is encouraged to review Malamed’s Handbook of Local Anesthesia.
IANB
As the name implies, this anesthetic technique anesthetizes the inferior alveolar nerve. The traditional technique as described by Malamed [2020] advises the use of a 27-gauge long needle. With the patient in a supine position and the mouth wide open, the needle approaches the target area from the contralateral side, with the syringe touching the contralateral corner of the mouth. Placing the index finger or thumb on the coronoid notch ipsilateral to the nerve to be anesthetized, the needle is inserted at 2/3 to 3/3 of the distance between the coronoid notch and the posterior border of the ramus, following an imaginary line parallel to the occlusal plane, towards the deepest part of the pterygomandibular raphe. This line usually is between 6 to 10 mm from the occlusal plane. The long needle penetrates 20 to 25 mm into the tissue, and 2–4 mL of the local anesthetic solution is injected (21,40). Although it is a commonly used technique, a high failure rate of up to 20% has been described. The failure is not limited to the experience of the administrator and does not seem to be related to the type of anesthetic given, which has highlighted the need for alternatives, such as the use of infiltration with 2% or 4% articaine for mandibular anesthesia (12,41).
IANB may require supplemental buccal nerve block when the buccal aspect of posterior soft tissue is involved or supplemental infiltration of incisive or mental nerves. Depending on the location of pain on the lower arch, an infiltration may be sufficient and preferable over the IANB. Lingual nerve block can be accomplished by delivering a few milliliters of anesthetic solution while retracting the needle after inferior alveolar nerve blockage.
Gow-Gates technique (Figure 5)

This technique anesthetizes all sensory terminal branches of the mandibular nerve, such as inferior alveolar, lingual, auriculotemporal and mylohyoid nerves. Buccal nerve may also be anesthetized, but not in all patients. The success rate of the Gow-Gates technique is very high with appropriate training (30).
The patient is placed in a supine or semi-supine position with mouth wide open. Using an imaginary line from the contralateral corner of the mouth and the lowest part of the tragus (inter-tragic notch), the insertion of the 25- or 27-gauge long needle is directed from the contralateral corner of the mouth towards the buccal mucosa distal to the maxillary second molar aiming to the lateral aspect of the neck of the condyle. The needle passes below the mesio-palatal cusp of the maxillary second molar (height of penetration) before going distally and penetrating the mucosa. The penetration should be slow until bone is touched, and 1.8 mL of local anesthetic should provide adequate anesthesia. The patient is then placed in upright position until the effect of the anesthesia is perceived (30).
Maxillary nerve block
Upon leaving the skull through the foramen rotundum, the maxillary nerve, the second division of the trigeminal nerve (V2) enters the pterygopalatine fossa. This is the precise location where a local anesthetic can be delivered to block V2 and its branches. Maxillary nerve consists of the main nerve trunks, such as the posterior and middle superior alveolar nerves, infra-orbital/anterior superior alveolar, greater and lesser palatine and nasopalatine nerves (30). When the anesthesia is performed more distally, at the terminal branches, it is termed as a field block. A field block is indicated when the area to be anesthetized is limited to one or two teeth and surrounding soft tissue. A field block can be achieved by supra-periosteal injection, described previously (42). A short 27-gauge needle can be used and placed parallel to the long axis of the tooth with the bevel directed toward the alveolar bone. The needle penetrates the muco-buccal fold to above the apex of the tooth, where the anesthetic solution is delivered.
There are two approaches to achieve the maxillary nerve block:
- The high tuberosity approach; the patient is in supine or semi-supine position, mouth slightly closed, chin moved to ipsilateral side of the nerve to be anesthetized. A long 25-gauge needle is inserted up to 30 mm depth from the muco-buccal fold above maxillary second molar, in an upward, inward and backward direction and aspiration must be performed before injecting the anesthetic solution.
- The greater palatine canal approach; with the patient also in supine position, with mouth wide open, the greater palatine foramen is located, with the bevel towards the tissue, and with an initial 45-degree angle, the needle is inserted into the canal to a depth of 30 mm to administer the solution. Needle aspiration is important. Bony obstructions are common inside the canal. In that case, a different approach is indicated. With this maxillary, or second division, nerve blocks, one half of the maxilla, excluding the most posterior part of the soft palate, is anesthetized (26).
Sphenopalatine ganglion block (Figure 6)
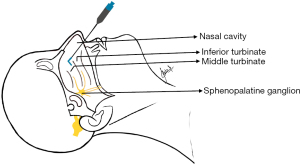
Acute attacks of TN, that are limited to the second branch of the trigeminal nerve, can be controlled for a few hours with sphenopalatine ganglion block. A safe technique, as compared to intravenous or intraoral injections, is to use 8% lidocaine spray (43), cotton saturated with 4% lidocaine, placed in the patient’s nose under endoscopic guidance (44), or by use of fluoroscopy guided injections in an inpatient setting (45). Anesthetic applicators indicated specifically for intranasal sphenopalatine blocks are available. Common side effects with this block include local burning, temporary anesthesia of the throat, nose and eye, ipsilateral lacrimation, and bitter taste (46).
Post-traumatic trigeminal neuropathic pain (PTNP)
According to the ICOP, this is unilateral or bilateral facial or oral pain, following and caused by trauma to the trigeminal nerve, persisting or recurring for more than 3 months. The pain levels in PTNP are usually moderate, but its constant unremitting feature is what makes it very distressing to patients. Occasionally, patients may present with allodynia, i.e., a painful response to a non-painful stimulus, where intense pain may be triggered by normal daily activities. In this situation, any of the blocks described for used for management of TN will be helpful here.
Another mechanism by which PTNP occurs is by the formation of a traumatic neuroma (47). When a nerve is severed, the proximal stump attempts to reconnect with the sectioned end, through regeneration. For this reconnection be successful, a conduit, naturally formed by Schwann cells, is required to guide this reconnection. When the reconnection is unsuccessful, the attempt of the nerve stump to reconnect results in a disorganized growth containing nerve fibers and fibrous tissue. The peripheral nerve endings within this “scar tissue” can be readily activated by inflammatory mediators and may produce spontaneous pain and hyperalgesia. Clinically neuroma pain is characterized as burning, possibly accompanied by paresthesia or anesthesia (48), and Tinel’s sign, which consists of eliciting sensation of tingling, or exacerbation of pain through local pressure of the neuroma.
Steroid injection into a traumatic neuroma
One technique for the management of a traumatic neuroma is to deliver an injection with local anesthesia mixed with steroids at the site. Generally, local anesthetic with epinephrine is not used, as it may sensitize the sympathetic nerve endings. Dexamethasone phosphate (4 mg/mL) solution is combined with local anesthetic such as mepivacaine without vasoconstrictor, and delivered intraorally at the site of the neuroma, which has been located by palpation of a ‘Tinel’s sign’. A small volume (0.1–0.4 cc) is sufficient to offer pain relief in recalcitrant pain cases.
Orofacial pains resembling presentations of primary headaches
The most common neurovascular orofacial pain emergencies are migraine and cluster headache.
Orofacial migraine
Migraine is a recurrent headache disorder, that lasts for 4–72 hours. Typically, the pain is located unilaterally, pulsating in quality, moderate to severe in intensity. It can be aggravated by routine physical activity. Associated features include nausea, photo and/or phonophobia (3).
For both episodic and chronic migraines, the greater occipital nerve block (GONB) has been shown to reduce pain (16,49). Complete pain resolution may be accomplished within 30 minutes after the injection, with sustained lower frequency of attacks (50).
GONB (Figure 7)

GONB is usually performed with a mixture of local anesthetic and steroids. With the patient in a prone or up-right position, the administrator localizes the midpoint between the external occipital protuberance and mastoid process through palpation. The target area for injection is 1 to 2 cm inferior to this point (51). The injection is usually performed at the most tender site within this location. A short 25-gauge needle perforates the skin and advances until it touches the periosteum. Then the needle is retrieved about 1 mm, aspiration is performed and administration of up to 3 mL of anesthetic solution is done. It is advised to apply pressure for about 1 minute at the site of injection once the needle is removed to reduce risk of hematoma and assist in spreading the anesthetic solution (40).
Sometimes, in combination with the GONB, supraorbital and supratrochlear nerve blocks, sphenopalatine ganglion blocks are indicated for acute migraines (6,14,52).
Supraorbital nerve block (Figure 8)
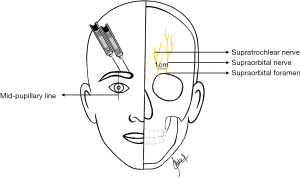
The supraorbital nerve exits the cranium through the supraorbital foramen located by palpation of the superior border of the orbit at the midpapillary line. The supraorbital nerve block is usually performed with a 27-gauge needle, in a lateral to medial direction, stopping before the entrance of the foramen. Following needle aspiration, 1 to 3 mL of local anesthetic is injected (14).
Supratrochlear nerve block (Figure 7)
The supratrochlear nerve exits the cranium within 1 cm medial of the supraorbital foramen. This nerve block is often performed in conjunction with the supraorbital nerve block, simply requiring a second injection placed slightly towards the facial midline (14).
The sphenopalatine ganglion block is also recommended for fast (within 15 minutes) of pain relief of acute attacks as described previously.
Orofacial cluster attack
This is a severe, strictly unilateral headache lasting 15–180 minutes and occurring once every other day to eight times a day. There is ipsilateral conjunctival injection, lacrimation, nasal congestion, rhinorrhea, forehead, and facial sweating, miosis, ptosis and or eyelid edema. The headache is accompanied with restlessness or agitation. Episodic and chronic cluster have been managed with GONB, combined with steroids (6,53). There is sustained pain relief after the injection, hence, this technique has been used for transitional therapy of chronic cluster headaches (54). A simple non-injectable technique is to use lidocaine drops into the eye, that have been used for abortion of cluster headaches, along with supratrochlear, supraorbital nerve blocks, and sphenopalatine ganglion blocks.
Summary
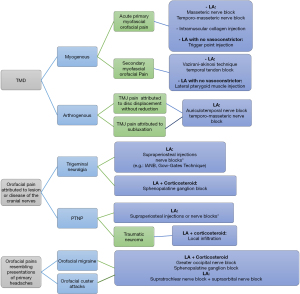
Injections can be very effective in the management of orofacial pain emergencies. They provide quick pain relief with minimal side effects and can be helpful while the patient is transitioning or is being titrated on systemic medications. A limitation of the present review is selection bias—as the authors were looking for articles on the injection techniques for orofacial pain emergencies. Future studies can look at the effectiveness of these techniques in managing orofacial pain emergencies. A flowchart (Figure 9) is presented at the end to serve as a guide. We hope this manuscript can serve as a guide for future research aiming to develop efficient techniques to alleviate the sufferings of patients with acute exacerbations of their orofacial pain conditions.
Acknowledgments
This work was supported by the Department of Diagnostic Sciences, Rutgers School of Dental Medicine.
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editor (Mythili Kalladka) for the series “Orofacial Pain: Diagnostic and Therapeutic Topicals, Nerve Blocks and Trigger Point Injection” published in Journal of Oral and Maxillofacial Anesthesia. The article has undergone external peer review.
Reporting Checklist: The authors have completed the Narrative Review reporting checklist. Available at https://joma.amegroups.com/article/view/10.21037/joma-22-11/rc
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://joma.amegroups.com/article/view/10.21037/joma-22-11/coif). The series “Orofacial Pain: Diagnostic and Therapeutic Topicals, Nerve Blocks and Trigger Point Injection” was commissioned by the editorial office without any funding or sponsorship. The authors have no other conflicts of interest to declare.
Disclaimer: The views expressed in this article are the authors’ own and not an official position of the Rutgers School of Dental Medicine.
Ethical Statement: The authors are accountable for all aspects of the work by ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Binaisse P, Dehours E, Bodéré C, et al. Dental emergencies at sea: A study in the French maritime TeleMedical Assistance Service. J Telemed Telecare 2020;26:285-93. [Crossref] [PubMed]
- AAOP. American Association of Orofacial Pain 2022. Available online: https://aaop.org/
- International Classification of Orofacial Pain, 1st edition (ICOP). Cephalalgia 2020;40:129-221.
- Okeson JP. Bell’s Orofacial Pains, 5th Edition: Quintesscence Books.
- Appasamy M, Lam C, Alm J, et al. Trigger Point Injections. Phys Med Rehabil Clin N Am 2022;33:307-33. [Crossref] [PubMed]
- Kleen JK, Levin M. Injection Therapy for Headache and Facial Pain. Oral Maxillofac Surg Clin North Am 2016;28:423-34. [Crossref] [PubMed]
- Moore PA, Hersh EV. Local anesthetics: pharmacology and toxicity. Dent Clin North Am 2010;54:587-99. [Crossref] [PubMed]
- Su N, Liu Y, Yang X, et al. Efficacy and safety of mepivacaine compared with lidocaine in local anaesthesia in dentistry: a meta-analysis of randomised controlled trials. Int Dent J 2014;64:96-107. [Crossref] [PubMed]
- Pogrel AM. Essentials of Oral and Maxillofacial Surgery. West Sussex, UK: Wiley Blackwell, 2014.
- Tal M. The effect of a long-acting local anaesthetic agent (Marcaine) on the masticatory muscle in rats. Int J Oral Surg 1982;11:101-5. [Crossref] [PubMed]
- Becker DE, Reed KL. Local anesthetics: review of pharmacological considerations. Anesth Prog 2012;59:90-101; quiz 102-3. [Crossref] [PubMed]
- Martin E, Nimmo A, Lee A, et al. Articaine in dentistry: an overview of the evidence and meta-analysis of the latest randomised controlled trials on articaine safety and efficacy compared to lidocaine for routine dental treatment. BDJ Open 2021;7:27. [Crossref] [PubMed]
- Zink W, Graf BM. Local anesthetic myotoxicity. Reg Anesth Pain Med 2004;29:333-40. [Crossref] [PubMed]
- Johnson AP, Boscoe E, Cabrera-Muffly C. Local Blocks and Regional Anesthesia in the Head and Neck. Otolaryngol Clin North Am 2020;53:739-51. [Crossref] [PubMed]
- Harbell MW, Bolton PB, Koyyalamudi V, et al. Evaluating the Anatomic Spread of Selective Nerve Scalp Blocks Using Methylene Blue: A Cadaveric Analysis. J Neurosurg Anesthesiol 2021; Epub ahead of print. [Crossref] [PubMed]
- Santos Lasaosa S, Cuadrado Pérez ML, Guerrero Peral AL, et al. Consensus recommendations for anaesthetic peripheral nerve block. Neurologia 2017;32:316-30. [Crossref] [PubMed]
- Vyvey M. Steroids as pain relief adjuvants. Can Fam Physician 2010;56:1295-7, e415.
- Jæger P, Grevstad U, Koscielniak-Nielsen ZJ, et al. Does dexamethasone have a perineural mechanism of action? A paired, blinded, randomized, controlled study in healthy volunteers. Br J Anaesth 2016;117:635-41. [Crossref] [PubMed]
- Nitecka-Buchta A, Walczynska-Dragon K, Batko-Kapustecka J, et al. Comparison between Collagen and Lidocaine Intramuscular Injections in Terms of Their Efficiency in Decreasing Myofascial Pain within Masseter Muscles: A Randomized, Single-Blind Controlled Trial. Pain Res Manag 2018;2018:8261090. [Crossref] [PubMed]
- De la Torre Canales G, Poluha RL, Lora VM, et al. Botulinum toxin type A applications for masticatory myofascial pain and trigeminal neuralgia: what is the evidence regarding adverse effects? Clin Oral Investig 2019;23:3411-21. [Crossref] [PubMed]
- DeAngelis AF, Barrowman RA, Harrod R, et al. Review article: Maxillofacial emergencies: oral pain and odontogenic infections. Emerg Med Australas 2014;26:336-42. [Crossref] [PubMed]
- Ananthan S, Subramanian G, Patel T, et al. The twin block injection: an adjunctive clinical aid for the management of acute arthrogenous temporomandibular joint dysfunction. Quintessence Int 2020;51:330-3. [PubMed]
- Warburton G. Internal Derangements of the Temporomandibular Joint. In: Bonanthaya K, Panneerselvam E, Manuel S, et al. editors. Oral and Maxillofacial Surgery for the Clinician. Singapore: Springer Singapore, 2021:1361-80.
- Chang CL, Wang DH, Yang MC, et al. Functional disorders of the temporomandibular joints: Internal derangement of the temporomandibular joint. Kaohsiung J Med Sci 2018;34:223-30. [Crossref] [PubMed]
- Zhou H, Xue Y, Liu P. Application of auriculotemporal nerve block and dextrose prolotherapy in exercise therapy of TMJ closed lock in adolescents and young adults. Head Face Med 2021;17:11. [Crossref] [PubMed]
- Quek SYP, Gomes-Zagury J, Subramanian G. Twin Block in Myogenous Orofacial Pain: Applied Anatomy, Technique Update, and Safety. Anesth Prog 2020;67:103-6. [Crossref] [PubMed]
- Ananthan S, Kanti V, Zagury JG, et al. The effect of the twin block compared with trigger point injections in patients with masticatory myofascial pain: a pilot study. Oral Surg Oral Med Oral Pathol Oral Radiol 2020;129:222-8. [Crossref] [PubMed]
- Quek SYP, Grunwerg BS. Masseteric nerve block for masseter muscle pain--a clinical note. Quintessence Int 2009;40:87-91. [PubMed]
- Bressler HB, Markus M, Bressler RP, et al. Temporal tendinosis: A cause of chronic orofacial pain. Curr Pain Headache Rep 2020;24:18. [Crossref] [PubMed]
- Malamed SF. Handbook of Local Anesthesia. Mosby, 2019.
- Khoury J, Townsend G. Neural blockade anaesthesia of the mandibular nerve and its terminal branches: rationale for different anaesthetic techniques including their advantages and disadvantages. Anesthesiol Res Pract 2011;2011:307423. [Crossref] [PubMed]
- Yang S, Exposto FG, Mahmoodi S, et al. Mechanical sensitivity changes in pericranial muscles after local anesthesia and experimentally induced pain in the temporalis tendon: Implications for headache and facial pain. Cephalalgia 2022; Epub ahead of print. [Crossref] [PubMed]
- Kucukguven A, Demiryurek MD, Kucukguven MB, et al. A Novel Injection Technique to the Lateral Pterygoid Muscle for Temporomandibular Disorders: A Cadaveric Study. Plast Reconstr Surg 2021;148:785e-90e. [Crossref] [PubMed]
- Koole P, Beenhakker F, de Jongh HJ, et al. A standardized technique for the placement of electrodes in the two heads of the lateral pterygoid muscle. Cranio 1990;8:154-62. [Crossref] [PubMed]
-
Terminology I. - Maarbjerg S, Gozalov A, Olesen J, et al. Trigeminal neuralgia--a prospective systematic study of clinical characteristics in 158 patients. Headache 2014;54:1574-82. [Crossref] [PubMed]
- Cruccu G. Trigeminal Neuralgia. Continuum (Minneap Minn) 2017;23:396-420. [Crossref] [PubMed]
- Moore D, Chong MS, Shetty A, et al. A systematic review of rescue analgesic strategies in acute exacerbations of primary trigeminal neuralgia. Br J Anaesth 2019;123:e385-96. [Crossref] [PubMed]
- Balta S, Köknel Talu G. Clinical effectiveness of peripheral nerve blocks with lidocaine and corticosteroid in patients with trigeminal neuralgia. Agri 2021;33:237-42. [Crossref] [PubMed]
- Shauly O, Gould DJ, Sahai-Srivastava S, et al. Greater Occipital Nerve Block for the Treatment of Chronic Migraine Headaches: A Systematic Review and Meta-Analysis. Plast Reconstr Surg 2019;144:943-52. [Crossref] [PubMed]
- Bartlett G, Mansoor J. Articaine buccal infiltration vs lidocaine inferior dental block - a review of the literature. Br Dent J 2016;220:117-20. [Crossref] [PubMed]
- Malamed S. Handbook of Local Anesthesia, Seventh Edition. Copyright @2020, Elsevier Inc., 2020;204-38 and 239-67.
- Mojica J, Mo B, Ng A. Sphenopalatine Ganglion Block in the Management of Chronic Headaches. Curr Pain Headache Rep 2017;21:27. [Crossref] [PubMed]
- Murty PS, Prasanna A. Endoscopic sphenopalatine ganglion block for pain relief. Indian J Otolaryngol Head Neck Surg 1998;50:99-105. [Crossref] [PubMed]
- Nagib M, Hood P, Matteo J. Sphenopalatine Ganglion Block: Treatment of Migraine and Trigeminal Neuralgia Associated With Multiple Sclerosis. Cureus 2020;12:e8522. [Crossref] [PubMed]
- Ho KWD, Przkora R, Kumar S. Sphenopalatine ganglion: block, radiofrequency ablation and neurostimulation - a systematic review. J Headache Pain 2017;18:118. [Crossref] [PubMed]
- Benoliel R, Kahn J, Eliav E. Peripheral painful traumatic trigeminal neuropathies. Oral Dis 2012;18:317-32. [Crossref] [PubMed]
- Rasmussen OC. Painful traumatic neuromas in the oral cavity. Oral Surg Oral Med Oral Pathol 1980;49:191-5. [Crossref] [PubMed]
- Flamer D, Alakkad H, Soneji N, et al. Comparison of two ultrasound-guided techniques for greater occipital nerve injections in chronic migraine: a double-blind, randomized, controlled trial. Reg Anesth Pain Med 2019;44:595-603. [Crossref] [PubMed]
- Friedman BW, Irizarry E, Williams A, et al. A Randomized, Double-Dummy, Emergency Department-Based Study of Greater Occipital Nerve Block With Bupivacaine vs Intravenous Metoclopramide for Treatment of Migraine. Headache 2020;60:2380-8. [Crossref] [PubMed]
- Afridi SK, Shields KG, Bhola R, et al. Greater occipital nerve injection in primary headache syndromes--prolonged effects from a single injection. Pain 2006;122:126-9. [Crossref] [PubMed]
- Tepper SJ, Caparso A. Sphenopalatine Ganglion (SPG): Stimulation Mechanism, Safety, and Efficacy. Headache 2017;57:14-28. [Crossref] [PubMed]
- Francis GJ, Becker WJ, Pringsheim TM. Acute and preventive pharmacologic treatment of cluster headache. Neurology 2010;75:463-73. [Crossref] [PubMed]
- Burish M. Cluster Headache and Other Trigeminal Autonomic Cephalalgias. Continuum (Minneap Minn) 2018;24:1137-56. [Crossref] [PubMed]
Cite this article as: Ananthan S, Quek SYP, Baddireddy SM, Gomes Zagury J. Use of injection techniques in orofacial pain emergencies: a narrative review. J Oral Maxillofac Anesth 2022;1:26.


