
肌筋膜源性颞下颌关节紊乱的实用管理——叙述性综述
引言
背景
咀嚼肌筋膜疼痛是颞下颌关节紊乱(temporomandibular disorder,TMD)最常见的类型,指的是源于下颌骨肌肉/肌筋膜和相关软组织的慢性疼痛。在美国,这一疾病影响了近500万人[1-3]。口颌面疼痛国际分类(International Classification of Orofacial Pain,ICOP)将咀嚼肌筋膜疼痛分为原发性和继发性两大类。
理论基础和知识空白
继发于急性软组织损伤和炎症的肌筋膜疼痛通常很容易诊断和处理,疼痛的缓解伴随着组织的愈合。然而,了解原发性咀嚼肌筋膜疼痛(在本文中称为“mTMD”)和组织愈合后疼痛持续存在的原因一直是研究中的难点[4-7]。
目的
本叙述性综述所涉及的关键问题有两个——对咀嚼肌源性TMD的病因和诊断的了解及管理。我们根据叙述性综述报告清单介绍以下文章(可在https://joma.amegroups.com/article/view/10.21037/joma-22-14/rc查看)。
方法
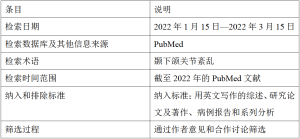
表1总结了本叙述性综述采用的研究方法。
Full table
讨论
目前对肌筋膜源性颞下颌关节紊乱的理解和管理基础
到目前为止,肌筋膜源性颞下颌关节紊乱(myofascial TMD,mTMD)的诊断主要依据患者的病史和临床检查[8]。在缺乏明确的组织病理学和任何定量评估证实临床诊断的情况下,医生的临床评估具有主观性和可变性。mTMD的特征之一是存在肌筋膜扳机点,也就是骨骼肌肌束中的压痛点,按压时会有牵涉痛[4,9]。在临床上,扳机点又分为活动性和潜伏性两类。两者在触诊时都有疼痛感,但只有前一种类型的扳机点能再现患者的疼痛主诉[5,9]。
肌筋膜疼痛的定义和病因尚不完全明确。mTMD疼痛的病理性扳机点引起了许多争论,包括它们是肌筋膜疼痛的结果还是原因,甚至它们是肌筋膜疼痛发生的必要条件还是充分条件这一点也值得商榷。事实上,针对肌筋膜疼痛的2020年美国国立卫生研究院(National Institutes of Health,NIH)的一次研讨会承认了这一重要问题的挑战性和由此带来的科研机遇[10]。学界提出了许多理论解释肌筋膜疼痛,但这些理论并未得到严格的验证。
一些关于原发性肌筋膜疼痛产生的假说认为,异常的肌肉负荷,如持续收缩或重复运动,或肌肉运动终板失灵,会导致无法自发释放从而致使乙酰胆碱积聚,导致外周炎症和潜在的组织损伤[11-15],还可能造成外周肌肉神经感受器和中枢敏化。
筋膜组织深入所有肌肉组织,与肌纤维密切接触,其广泛的神经支配有助于肌筋膜疼痛的病理生理学研究[10]。肌筋膜单元假说认为筋膜组织是肌筋膜疼痛发病机制中的一个重要因素。筋膜组织内有肌梭和高尔基体,并含有游离神经末梢,在某些情况下能够传递疼痛[16]。随着年龄的增长,人体筋膜组织不断发生变化,并受性激素和内分泌的影响,这与mTMD的风险因素相一致,如年龄增长、女性、情绪/心理压力[3,17]。外周敏化的临床表现包括颌骨活动时产生的疼痛或因局部按压导致疼痛加剧[11,12,15]。
中枢神经系统的伤害性感受神经元对敏化的外周传入神经的敏感性持续增加,可能导致继发性传入神经过度兴奋,这种现象也被称为中枢敏化,并且可以解释mTMD的疼痛,如自发性疼痛和牵涉痛[18,19]。
可以理解,这些理论都是成立的,肌筋膜疼痛的发病机制为多种机制的组合。因此,咀嚼肌筋膜疼痛的病因学可能是多因素的。咀嚼肌筋膜疼痛可以主要表现为局限于咀嚼肌筋膜组织的“局部”现象,也可以表现为涉及中枢神经系统层面的“广泛”现象。这些表现在“口颌面疼痛:前瞻性评估和风险评估(Orofacial Pain: Prospective Evaluation and Risk Assessment,OPPERA)研究”中都曾观察到过[3,17]。
慢性疼痛中的mTMDs
OPPERA研究是一项开创性的、基于多人群的前瞻性研究,旨在确定导致TMD发病和持续存在的风险因素。经确定,这些风险因素为生物−心理−社会、环境或遗传因素[20]。患有TMD的受试者自我报告的一些因素包括下颌外伤、行为功能异常、面部和下颌的疼痛强度加剧、下颌运动导致疼痛改变、僵硬或痉挛、关节弹响、头痛,甚至身体其他部位的慢性疼痛[3,17]。
值得注意的是,剧烈疼痛,即高强度的疼痛或自我报告的中度/高度疼痛相关的影响,在口颌面疼痛患者中的发生率比非口颌面疼痛者高近4倍。此外,剧烈疼痛的患者对疼痛敏感度更高,触压身体多个部位时有更明显的压痛感[3,17,21]。
慢性TMD患者的社会心理风险因素包括更高层级的心理和情感问题、更强烈的压力感知和灾难化思维,以及更丰富的躯体意识[22]。
OPPERA研究对有较高风险发展为疼痛性TMD的个体进行了分组——适应性群组、疼痛敏感群组和整体症状群组。适应性群组中的个体局部病变更多,而其他两个群组中的个体则被认为由于中枢敏化而疼痛敏感性更高[23]。
这些数据表明,mTMD既可能是一种单独的表现,也可能是机制更“广泛”或“集中”的现象群的一部分。因此,TMD疼痛常常与偏头痛、纤维肌痛和其他类型的全身性疼痛合并。
mTMDs的管理
管理肌筋膜疼痛的方法有很多,干针疗法、扳机点注射、口腔矫治器、针灸和软组织松解术等,这里仅举几例[24,25]。最近一项关于肌源性TMD治疗方法的系统综述的荟萃分析表明,最有效的治疗方法是手法治疗、咨询、局部麻醉(扳机点注射)和矫治器治疗,但这一结论存在较大程度的争议,主要是由于方法的异质性。这导致大多数治疗方法的证据水平较低,研究质量需要提升[26,27]。
咨询和自我护理
咨询的内容可以包括从有关病情、预后和自我护理技巧的患者教育,到更具体的认知行为疗法(cognitive-behavioral therapy,CBT)。咨询通常与其他治疗方法相结合,对急性和慢性疾病都有积极作用[28]。
口腔矫治器
口腔矫治器是治疗mTMD最常见的手段[27]。文献中描述了多种类型的口腔矫治器。建议使用深覆盖丙烯酸硬质矫治器,覆盖上颌或下颌牙弓,双侧中心接触对侧牙齿,长期使用以减少咬合的变化。但这类矫治器的缺点是成本高、制作时间长、需要定期维护,最重要的是要注意矫治器是否合适以及指导患者正确使用[25,29]。
物理治疗
组织操作,也称为手法操作或治疗,包括对头颈部软组织和关节的操作。有不同的技术,一般期望的结果包括改善肌肉痉挛、局部循环和粘连,增加运动范围,改善疼痛。这种疗法需要由物理治疗师进行多次治疗[30,31]。
扳机点注射
在骨骼肌肌束扳机点注射不含血管收缩药的局部麻醉药[13]。系统综述的网络荟萃分析发现,扳机点注射局部麻醉药可以缓解疼痛,同时改善最大张口度至少6个月[32]。扳机点注射的技术要求高,需要准确的诊断、定位和操作[33]。
干针疗法
干针疗法是一种治疗肌筋膜疼痛的方法,通常由物理治疗师进行,将实心细针扎入肌筋膜扳机点、肌腱、韧带和疤痕组织[34]。这种方式被认为可以缓解外周疼痛和敏化[29]。
针灸
针灸是中医的一种治疗方式,在特定的位置,也就是穴位,扎入多根实心细针。这一方法由受过训练的专业人员操作,需要定期随访。多种针灸方法被认为可以改善疼痛和由其导致的张口受限,提高生活质量[35]。由于针灸对mTMD疗效的证据有限,因此针灸被认为是mTMD治疗的辅助手段[24]。
此外,口服药物治疗这类疼痛的方法也逐渐获得支持,如普瑞巴林[36]。
目前,该领域在验证各种治疗方式的相对有效性方面存在空白,这一点并不能通过对现有文献进行更多的批判性评估,即在已有文献的基础上进行更多的系统综述或荟萃分析弥补。从本文中可以推断出,已经进行并发表了多项这类分析,但与之相反的是,目前缺乏随机、多盲(操作者、评估者和受试者)的临床试验对有前景的治疗方式进行严格设计的前瞻性比较,这类临床试验能够对患者进行客观的评估、无偏见的治疗分配和结果评估。在这类试验发表之前,探索其他策略也有意义,这些策略适用于简单的治疗方法和更明确的患者反应评估。最近,我们发现了一种新的治疗方法——颞-咬肌神经阻滞(temporo-masseteric nerve block,TMNB),过去称之为双阻滞[37-41]。
TMNB作为管理mTMD的新工具
TMNB是一种局部麻醉注射技术,目标是三叉神经,即第五对脑神经,下颌支(V3)的颞深神经和咬肌神经(图1)[40,41]。TMNB研究的原动力是这样一种观点:中断来自肌肉的疼痛信号的传递可以缓解患者的疼痛症状,无论疼痛的起源是肌肉中的扳机点还是周围的软组织。此外,有选择地中断面部肌肉的神经支配有助于区分咀嚼肌源性疼痛和牙源性疼痛,在遇到疼痛来源难以定位的患者时,可以借此理清疼痛来源[42]。
我们观察到TMNB的疼痛缓解效果往往持续数周至数月,远远超过了局部麻醉药本身的作用时间(作者的临床观察)。这表明了一种可能性,即TMNB可能有治疗咬肌和(或)颞肌疼痛的价值。TMNB缓解疼痛的机制尚待研究;我们推测,由于支配咬肌和颞肌的神经是混合神经(感觉和运动),给予局部麻醉药会影响肌肉的运动。这可能反过来中断与慢性疼痛有关的“疼痛—同步收缩—疼痛”循环,从而使疼痛的缓解时间比局部麻醉药的作用时间长。
虽然TNMB介导的持续缓解疼痛的机制尚未明确,但有数据证实其在缓解弥漫性肌筋膜炎方面的功效[37,39]。TMNB缓解疼痛的效果与扳机点注射相当,可持续6个月[37]。这有两方面的意义。首先,识别扳机点的能力需要经过专门的培训才能掌握,而普通牙医不具备这种能力。因此,患有慢性咀嚼肌筋膜疼痛的患者常常被误诊,或被多次转诊,导致治疗延误。但TMNB容易实践,只需普通医生可以随时获得的牙科麻醉药和注射器。其次,它不需要确定扳机点,因此有可能将咀嚼肌筋膜疼痛转变为普通医生可以轻易诊断和治疗的疾病。
需要解决的关键问题是TMNB的安全性。在过去7年中,TMNB已被用于临床,且没有任何关于其使用后出现短期或持续不良反应的报告(文章正在准备中)[43]。这一牙科麻醉技术已在全球范围内常规使用,因此其安全性已得到充分证实。
TMNB作为“分类器”将mTMD分为外周和中枢现象?
我们推测,当发病机制集中在局部时,像TMNB这样的外周干预措施在评估或管理咀嚼肌筋膜疼痛(mTMD)方面可能特别有效。同时,也可以通过评估TMNB的治疗效果来识别/界定那些可能为中枢机制引起的肌筋膜疼痛的患者。这一技术对于识别那些需要多学科加强护理的患者可能至关重要,但目前还没有数据支持这一观点,这只是一种假设。然而,我们的结论是,由于mTMD患者临床表现的复杂性和异质性,进行这种研究是有必要的。
优势和不足
本文对文献进行了严格的评估,提出了管理mTMD的新观点,并推荐将TMNB作为一种可能的干预措施。TMNB简单易行且患者的耐受性良好。但需要注意的是,这一观点仅为推测,TMNB方法还需进一步验证。
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editor (Mythili Kalladka) for the series “Orofacial Pain: Diagnostic and Therapeutic Topicals, Nerve Blocks and Trigger Point Injection” published in Journal of Oral and Maxillofacial Anesthesia. The article has undergone external peer review.
Reporting Checklist: The authors have completed the Narrative Review reporting checklist. Available at https://joma.amegroups.com/article/view/10.21037/joma-22-14/rc
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://joma.amegroups.com/article/view/10.21037/joma-22-14/coif). The series “Orofacial Pain: Diagnostic and Therapeutic Topicals, Nerve Blocks and Trigger Point Injection” was commissioned by the editorial office without any funding or sponsorship. GS declares that granted with institutional support, and presented CE and received payment (Dec 2020) from Physicians’ Education Resource®, LLC (PER®) for CME program, titled Clinical Consultations™: Improving the Coordination of Care Between Dentists, Oral Surgeons, and Osteoporosis Specialists to Reduce the Risk of ONJ. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Von Korff M, Dworkin SF, Le Resche L, et al. An epidemiologic comparison of pain complaints. Pain 1988;32:173-83. [Crossref] [PubMed]
- Isong U, Gansky SA, Plesh O. Temporomandibular joint and muscle disorder-type pain in U.S. adults: the National Health Interview Survey. J Orofac Pain 2008;22:317-22. [PubMed]
- Bair E, Brownstein NC, Ohrbach R, et al. Study protocol, sample characteristics, and loss to follow-up: the OPPERA prospective cohort study. J Pain 2013;14:T2-19. [Crossref] [PubMed]
- Duarte FCK, West DWD, Linde LD, et al. Re-Examining Myofascial Pain Syndrome: Toward Biomarker Development and Mechanism-Based Diagnostic Criteria. Curr Rheumatol Rep 2021;23:69. [Crossref] [PubMed]
- Fricton J. Myofascial Pain: Mechanisms to Management. Oral Maxillofac Surg Clin North Am 2016;28:289-311. [Crossref] [PubMed]
- Cao QW, Peng BG, Wang L, et al. Expert consensus on the diagnosis and treatment of myofascial pain syndrome. World J Clin Cases 2021;9:2077-89. [Crossref] [PubMed]
- Prodoehl J, Kraus S, Klasser GD, et al. Temporomandibular disorder content in the curricula of physical therapist professional programs in the United States. Cranio 2020;38:376-88. [Crossref] [PubMed]
- Schiffman E, Ohrbach R, Truelove E, et al. Diagnostic Criteria for Temporomandibular Disorders (DC/TMD) for Clinical and Research Applications: recommendations of the International RDC/TMD Consortium Network and Orofacial Pain Special Interest Group. J Oral Facial Pain Headache 2014;28:6-27. [Crossref] [PubMed]
- Bron C, Dommerholt JD. Etiology of myofascial trigger points. Curr Pain Headache Rep 2012;16:439-44. [Crossref] [PubMed]
- NIH. Quantitative Evaluation of Myofascial Tissues: Potential Impact for Musculoskeletal Pain Research. 2020.
- Vardeh D, Mannion RJ, Woolf CJ. Toward a Mechanism-Based Approach to Pain Diagnosis. J Pain 2016;17:T50-69. [Crossref] [PubMed]
- Jafri MS. Mechanisms of Myofascial Pain. Int Sch Res Notices 2014;2014:523924. [Crossref] [PubMed]
- Gerwin RD. Myofascial Trigger Point Pain Syndromes. Semin Neurol 2016;36:469-73. [Crossref] [PubMed]
- Gerwin RD, Dommerholt J, Shah JP. An expansion of Simons' integrated hypothesis of trigger point formation. Curr Pain Headache Rep 2004;8:468-75. [Crossref] [PubMed]
- Woźniak K, Lipski M, Lichota D, et al. Muscle fatigue in the temporal and masseter muscles in patients with temporomandibular dysfunction. Biomed Res Int 2015;2015:269734. [Crossref] [PubMed]
- Stecco A, Gesi M, Stecco C, et al. Fascial components of the myofascial pain syndrome. Curr Pain Headache Rep 2013;17:352. [Crossref] [PubMed]
- Fillingim RB, Slade GD, Greenspan JD, et al. Long-term changes in biopsychosocial characteristics related to temporomandibular disorder: findings from the OPPERA study. Pain 2018;159:2403-13. [Crossref] [PubMed]
- Fernández-de-las-Peñas C, Dommerholt J. Myofascial trigger points: peripheral or central phenomenon? Curr Rheumatol Rep 2014;16:395. [Crossref] [PubMed]
- Ji RR, Nackley A, Huh Y, et al. Neuroinflammation and Central Sensitization in Chronic and Widespread Pain. Anesthesiology 2018;129:343-66. [Crossref] [PubMed]
- Maixner W, Diatchenko L, Dubner R, et al. Orofacial pain prospective evaluation and risk assessment study--the OPPERA study. J Pain 2011;12:T4-11.e1-2.
- National Academies of Sciences, Engineering, and Medicine; Health and Medicine Division; Board on Health Care Services; Board on Health Sciences Policy; Committee on Temporomandibular Disorders (TMDs): From Research Discoveries to Clinical Treatment, Yost O, Liverman CT, English R, et al. editors. Temporomandibular Disorders: Priorities for Research and Care. Washington (DC): National Academies Press (US); 2020.
- Fillingim RB, Ohrbach R, Greenspan JD, et al. Potential psychosocial risk factors for chronic TMD: descriptive data and empirically identified domains from the OPPERA case-control study. J Pain 2011;12:T46-60. [Crossref] [PubMed]
- Bair E, Gaynor S, Slade GD, et al. Identification of clusters of individuals relevant to temporomandibular disorders and other chronic pain conditions: the OPPERA study. Pain 2016;157:1266-78. [Crossref] [PubMed]
- Kalladka M, Young A, Khan J. Myofascial pain in temporomandibular disorders: Updates on etiopathogenesis and management. J Bodyw Mov Ther 2021;28:104-13. [Crossref] [PubMed]
- Al-Moraissi EA, Wolford LM, Ellis E 3rd, et al. The hierarchy of different treatments for arthrogenous temporomandibular disorders: A network meta-analysis of randomized clinical trials. J Craniomaxillofac Surg 2020;48:9-23. [Crossref] [PubMed]
- Feng J, Luo M, Ma J, et al. The treatment modalities of masticatory muscle pain a network meta-analysis. Medicine (Baltimore) 2019;98:e17934. [Crossref] [PubMed]
- Al-Moraissi EA, Farea R, Qasem KA, et al. Effectiveness of occlusal splint therapy in the management of temporomandibular disorders: network meta-analysis of randomized controlled trials. Int J Oral Maxillofac Surg 2020;49:1042-56. [Crossref] [PubMed]
- Noma N, Watanabe Y, Shimada A, et al. Effects of cognitive behavioral therapy on orofacial pain conditions. J Oral Sci 2020;63:4-7. [Crossref] [PubMed]
- Fernandes G, Gonçalves DAG, Conti P. Musculoskeletal Disorders. Dent Clin North Am 2018;62:553-64. [Crossref] [PubMed]
- Calixtre LB, Moreira RF, Franchini GH, et al. Manual therapy for the management of pain and limited range of motion in subjects with signs and symptoms of temporomandibular disorder: a systematic review of randomised controlled trials. J Oral Rehabil 2015;42:847-61. [Crossref] [PubMed]
- Bialosky JE, Bishop MD, Price DD, et al. The mechanisms of manual therapy in the treatment of musculoskeletal pain: a comprehensive model. Man Ther 2009;14:531-8. [Crossref] [PubMed]
- Al-Moraissi EA, Alradom J, Aladashi O, et al. Needling therapies in the management of myofascial pain of the masticatory muscles: A network meta-analysis of randomised clinical trials. J Oral Rehabil 2020;47:910-22. [Crossref] [PubMed]
- Hammi C, Schroeder JD, Yeung B. Trigger Point Injection. Treasure Island (FL): StatPearls Publishing; July 25, 2022.
- Dunning J, Butts R, Mourad F, et al. Dry needling: a literature review with implications for clinical practice guidelines. Phys Ther Rev 2014;19:252-65. [Crossref] [PubMed]
- Serritella E, Galluccio G, Impellizzeri A, et al. Comparison of the Effectiveness of Three Different Acupuncture Methods for TMD-Related Pain: A Randomized Clinical Study. Evid Based Complement Alternat Med 2021;2021:1286570. [Crossref] [PubMed]
- Karamanlioglu DS, Geler Kulcu D, Ozturk G, et al. Effectiveness of pregabalin treatment for trigger points in patients with comorbid myofascial pain syndrome and fibromyalgia syndrome: a randomized controlled trial. Somatosens Mot Res 2021;38:327-32. [Crossref] [PubMed]
- Ananthan S, Kanti V, Zagury JG, et al. The effect of the twin block compared with trigger point injections in patients with masticatory myofascial pain: a pilot study. Oral Surg Oral Med Oral Pathol Oral Radiol 2020;129:222-8. [Crossref] [PubMed]
- Ananthan S, Subramanian G, Patel T, et al. The twin block injection: an adjunctive clinical aid for the management of acute arthrogenous temporomandibular joint dysfunction. Quintessence Int 2020;51:330-3. [PubMed]
- Kanti V, Ananthan S, Subramanian G, et al. Efficacy of the twin block, a peripheral nerve block for the management of chronic masticatory myofascial pain: A case series. Quintessence Int 2017; Epub ahead of print. [Crossref] [PubMed]
- Quek S, Young A, Subramanian G. The twin block: a simple technique to block both the masseteric and the anterior deep temporal nerves with one anesthetic injection. Oral Surg Oral Med Oral Pathol Oral Radiol 2014;118:e65-7. [Crossref] [PubMed]
- Quek SYP, Gomes-Zagury J, Subramanian G. Twin Block in Myogenous Orofacial Pain: Applied Anatomy, Technique Update, and Safety. Anesth Prog 2020;67:103-6. [Crossref] [PubMed]
- Quek SYP, Kalladka M, Kanti V, et al. A new adjunctive tool to aid in the diagnosis of myogenous temporomandibular disorder pain originating from the masseter and temporalis muscles: Twin-block technique. J Indian Prosthodont Soc 2018;18:181-5. [Crossref] [PubMed]
- Makhija D, Quek SYP, Subramanian G. The Twin Block Safely and Effectively Alleviates Masticatory Myogenous Pain. 2021 IADR/AADR/CADR General Session (Virtual Experience). 2021.

夏明
上海交通大学医学院附属第九人民医院麻醉科副主任医师,副教授,硕士研究生导师,人工智能课题组长。Journal of Medical Artificial Intelligence(JMAI)主编,Journal of Oral and Maxillofacial Anesthesia(JOMA)执行主编,中华口腔医学会口腔麻醉专业委员会全国常务委员,中华口腔医学会镇静镇痛专委会全国常务委员,中国康复医学会疼痛康复专委会全国委员。(更新时间:2023-02-17)
(本译文仅供学术交流,实际内容请以英文原文为准。)
Cite this article as: Subramanian G, Ananthan S, Zagury JG, Quek SYP. Pragmatic management of myogenous temporomandibular disorder—a narrative review. J Oral Maxillofac Anesth 2022;1:35.




